Niyati Parekh

Niyati Parekh
Professor of Public Health Nutrition
Associate Vice Provost for Faculty Initiatives and Global Engagement, Office of the Provost
-
Professional overview
-
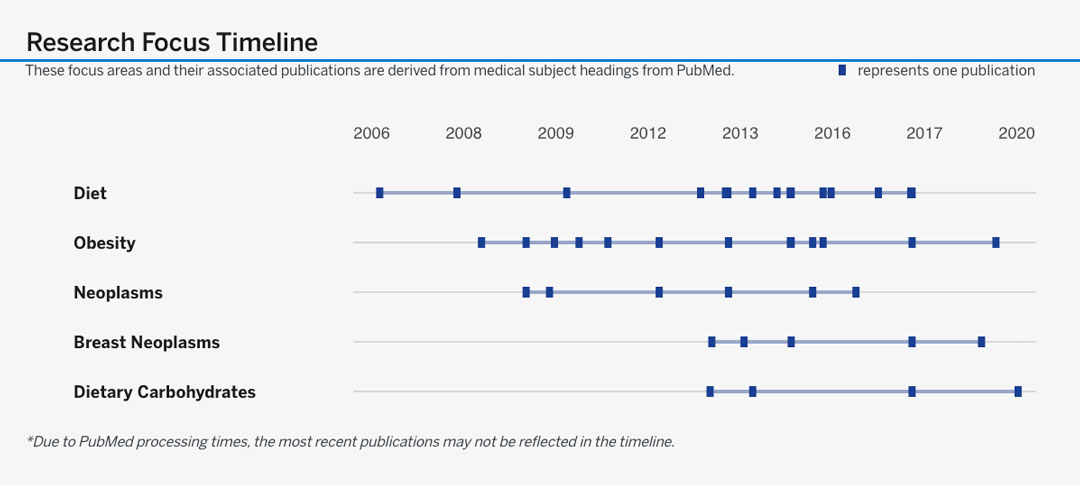
Dr. Niyati Parekh’s research and teaching are motivated by a deep commitment to reduce nutrition-related disease outcomes in at-risk groups. In pursuit of this goal, as a nutritional epidemiologist, she has developed a robust research portfolio that examines the intersection of biological and behavioral factors of non-communicable diseases in US populations. The overarching theme of her research program is to examine the role of nutrition and diet-related factors in the etiology of non-communicable diseases, with a particular focus on obesity, metabolic dysregulation and cancer. Her multidisciplinary research integrates the intricacies from four distinct areas of expertise: disease biology, nutritional biochemistry, epidemiology and biostatistics. She has developed a research program with three interconnected areas that are unified under the theme of investigating diet and non-communicable diseases in populations, using epidemiologic methods. The first arm consists of leveraging existing data to identify dietary patterns, dietary quality and food consumption patterns in populations of interest. The second is to identify dietary determinants and biomarkers that predict disease outcomes including obesity, diabetes, cardiovascular disease and cancer. The third arm is to measure diets using novel dietary assessment methods that will contribute to more accurate and multi-dimensional measurement of diet. The three areas of her work complement each other and reveal preventive measures for populations, inform health policy and guide clinical practice. She has 75 peer-reviewed publications and her work has been supported by awards from the American Cancer Society and NIH.
Dr. Parekh holds an MS in Clinical Nutrition from Mumbai University and a PhD in Nutritional Sciences with a minor in Population Health Sciences from the University of Wisconsin-Madison (2005). After completing a 2-year postdoctoral fellowship in Cancer Epidemiology at the Cancer Institute of New Jersey-Rutgers, she joined New York University Steinhardt’s Department of Nutrition, Food Studies and Public Health in January 2008. With doctoral and postdoctoral training in epidemiological methods, she cross-pollinated the fields of nutrition and public health. In 2015, as Associate Professor of Public Health Nutrition, she transitioned to NYU’s newly launched School of Global Public Health (GPH), as Director of the Public Health Nutrition program (until 2019). She also has an affiliated appointment at the Department of Population Health-Grossman School of Medicine.
Her recent honors include being inducted as a New York Academy of Medicine Fellow, and her appointment as Independent Consultant at UNICEF. She has served the American Society for Nutrition as Chair of the Nutritional Epidemiology Research Group. She teaches graduate courses in the New York Campus and at study abroad sites (Mexico, Abu Dhabi and Florence). Graduate courses taught include Global Nutrition, Nutritional Epidemiology, Perspectives in Public Health and Global Cancer Epidemiology for which she has received awards. Dr. Parekh has served as the Executive Director of Doctoral Programs at GPH since 2017. In this role, she supports about 30 PhD students, and promotes all aspects of their rigorous research and professional development towards impactful careers.
-
Education
-
BS, Life Sciences and Biotechnology, Mumbai University, IndiaMS, Foods, Nutrition, and Clinical Dietetics, Mumbai University, IndiaPhD, Nutritional Sciences (minor Population Health Sciences), University of Wisconsin-Madison, Madison, WI
-
Areas of research and study
-
CancerChronic DiseasesEpidemiologyNutritionObesityPopulation HealthPublic Health Nutrition
-
Publications
Publications
Association between behavioural risk factors for hypertension and concordance with the Dietary Approaches to Stop Hypertension dietary pattern among South Asians in the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study
AbstractHussain, B. M., Deierlein, A. L., Kanaya, A. M., Talegawkar, S. A., O’Connor, J. A., Gadgil, M. D., Needham, B. L., Lin, Y., & Parekh, N. (n.d.).Publication year
2025Journal title
Journal of Nutritional ScienceVolume
14AbstractSouth Asians are among the fastest-growing immigrant population group in the United States (U.S.) with a unique disease risk profile. Due in part to immigration and acculturation factors, South Asians engage differently with behavioural risk factors (e.g. smoking, alcohol intake, physical activity, sedentary behaviour, and diet) for hypertension, which may be modified for the primary prevention of cardiovascular disease. Using data from the Mediators of Atherosclerosis in South Asians Living in America cohort, we conducted a cross-sectional analysis to evaluate the association between behavioural risk factors for cardiovascular disease and diet. We created a behavioural risk factor score based on smoking status, alcohol consumption, physical activity, and TV watching. We also calculated a Dietary Approaches to Stop Hypertension (DASH) dietary score based on inclusion of relevant dietary components. We used both scores to examine the association between engaging with risk factors for hypertension and the DASH diet among a cohort of South Asian adults. We found that participants with 3–4 behavioural risk factors had a DASH diet score that was 3 units lower than those with no behavioural risk factors (aβ: –3.25; 95% CI: –4.28, –2.21) and were 86% less likely to have a DASH diet score in the highest category compared to the lowest DASH diet score category (aOR: 0.14; 95% CI: 0.05, 0.37) in the fully adjusted models. These findings highlight the relationship between behavioural risk factors for hypertension among South Asians in the U.S.Cardiovascular Health in the Transition From Adolescence to Emerging Adulthood : A Scientific Statement From the American Heart Association
AbstractAmerican Heart Association Prevention Science Committee of the Council on Epidemiology Prevention Council on Cardiovascular Stroke Nursing, A., Council on Lifelong Congenital Heart Disease Heart Health in the Young and Council on Lifestyle Cardiometabolic Health, A., Scott, J., Agarwala, A., Baker-Smith, C. M., Feinstein, M. J., Jakubowski, K., Kaar, J., Parekh, N., Patel, K. V., & Stephens, J. (n.d.).Publication year
2025Journal title
Journal of the American Heart AssociationVolume
14Issue
9AbstractCardiovascular disease remains a leading cause of death in the United States, with an alarming rise in the proportion of young adults experiencing cardiovascular events. Many adolescents enter adulthood with significant cardiovascular disease risk factors. This scientific statement addresses the critical need for cardiovascular health promotion during emerging adulthood, a transitional stage between the ages of 18 and 25 or 29 years of age. We discuss the significance of social determinants of health and the interplay between individual-level risk factors and developmental changes, including shifts in substance use, social connections, and emotional well-being. We conclude by outlining strategies for optimizing cardiovascular health promotion and disease prevention, underscoring the importance of primordial prevention, early intervention, and tailored approaches to address the unique needs of emerging adults. Addressing these multifaceted factors is crucial for mitigating the burden of cardiovascular disease risk factors among emerging adults and promoting long-term cardiovascular well-being.Concordance Between DASH Diet and Coronary Artery Calcification : Results From the Mediators of Atherosclerosis in South Asians Living in America (MASALA) Prospective Cohort Study
AbstractHussain, B. M., Deierlein, A. L., Talegawkar, S. A., Kanaya, A. M., O'Connor, J. A., Gadgil, M. D., Lin, Y., & Parekh, N. (n.d.).Publication year
2025Journal title
AJPM FocusVolume
4Issue
1AbstractIntroduction: South Asian adults are at high risk for atherosclerotic cardiovascular disease, for which coronary artery calcification is an early predictor. Adherence to the Dietary Approaches to Stop Hypertension diet is a modifiable risk factor that may mitigate the progression of coronary artery calcification and atherosclerotic cardiovascular disease. Methods: Using data from the Mediators of Atherosclerosis in South Asians Living in America cohort, the authors calculated a Dietary Approaches to Stop Hypertension dietary score (categorized as low, moderate, and high) to examine the associations of Dietary Approaches to Stop Hypertension diet adherence with coronary artery calcification after a 5-year follow up. Results: The authors found that participants in the high Dietary Approaches to Stop Hypertension category were 41% less likely to have coronary artery calcification score >100 (age-adjusted incidence rate ratio=0.59; 95% CI=0.36, 0.95) than those in the low category; this association was attenuated in multivariable models. Differences were observed by sex. Men in the high Dietary Approaches to Stop Hypertension category were 51% less likely to have coronary artery calcification score >100 (adjusted incidence rate ratio=0.49; 95% CI=0.26, 0.95) and experienced 0.46-fold coronary artery calcification change (fold change=0.46; 95% CI=0.18, 0.90) in multivariable models. Conclusions: The findings indicate a relationship between Dietary Approaches to Stop Hypertension diet and early predictors of atherosclerotic cardiovascular disease risk among South Asians living in the U.S., particularly men.The role of ultra-processed food in obesity
AbstractJuul, F. C., Martinez-Steele, E., Parekh, N., & Monteiro, C. A. (n.d.).Publication year
2025Journal title
Nature Reviews EndocrinologyAbstractThe global increase in obesity has occurred in parallel to a dietary shift from traditional staple foods to ultra-processed foods (UPF), spurring scientific interest in UPF as a driver of the obesity pandemic. Herein, we summarize the current evidence regarding the role of UPF in obesity, with a specific focus on potential biological mechanisms. The literature strongly supports and corroborates ecological, epidemiological and mechanistic lines of research indicating that dietary patterns high in UPF promote overeating and increase the risk of overweight and obesity. Experimental evidence demonstrates that the soft texture, high energy density and hyperpalatable nutrient combinations of UPF facilitate excessive energy intakes by affecting ingestive behaviours, satiety signalling and food reward systems. Although not fully elucidated, it is plausible that several other UPF attributes (such as emulsifiers, non-nutritive sweeteners, acellular nutrients, and contaminants from processing and packaging materials) contribute to their obesogenic effects through a myriad of physiological pathways, including altered absorption kinetics, glycaemic response and the gut microbiota composition and function. To stem the global rise in obesity, multipronged policy efforts are needed to reduce UPF consumption and create health-promoting food systems.Dietary patterns in the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study : Comparisons across methodologies
AbstractBeasley, J. M., Hussain, B. M., Gadgil, M. D., Talegawkar, S. A., Parekh, N., Bhupathiraju, S. N., Islam, N. S., & Kanaya, A. M. (n.d.).Publication year
2024Journal title
BMJ Nutrition, Prevention and HealthAbstract~Personal and Social-Built Environmental Factors of Glucose Variability Among Multiethnic Groups of Adults With Type 2 Diabetes : Research Protocol Using Ecological Momentary Assessment, Continuous Glucose Monitoring, and Actigraphy
AbstractNam, S., Jeon, S., Ash, G. I., Weinzimer, S., Dunton, G. F., Parekh, N., Grey, M., Chen, K., Lee, M., Sajdlowska, A., & Whittemore, R. (n.d.).Publication year
2024Journal title
Research in Nursing and HealthVolume
47Issue
6Page(s)
608-619AbstractGlucose variability (GV)—the degree of fluctuation in glucose levels over a certain period of time—is emerging as an important parameter of dynamic glycemic control. Repeated glycemic oscillations have been reported to be the link to diabetes complications. This prospective observational study aims to: (1) identify multilevel risk factors (personal and social-built environmental factors) associated with high GV; (2) identify “within-person predictors” of high GV leveraging the intra-person data to inform future personalized diabetes interventions; and (3) examine which lifestyle factors either mediate or moderate the relationship between emotional well-being and GV among diverse adults with type 2 diabetes (T2D). We will recruit 200 adults with T2D from the community. All participants will complete baseline surveys assessing demographics, lifestyle, social-built environmental, and clinical factors. Real-time dynamic glucose levels will be measured using continuous glucose monitoring (CGM). Sleep, physical activity, diet/eating, and emotional well-being will be measured with an actigraphy device and a real-time self-report tool (ecological momentary assessment [EMA]) across 14 days. Two 24-h dietary recall data will be collected by online video calls. Generalized linear models, multilevel models, and structural equation models will be developed to achieve the study aims. The findings from the study will identify high-risk groups of high GV who would benefit from CGM to improve diabetes outcomes and inform the future development of personalized just-in-time interventions targeting lifestyle behaviors with an increased understanding of GV and by supporting healthcare providers' clinical decisions.Ultra-processed food intake among South Asians in the United States : Specific vulnerabilities of a growing immigrant population group
AbstractHussain, B. M., Juul, F. C., Deierlein, A. L., & Parekh, N. (n.d.).Publication year
2024Journal title
Nutrition ReviewsVolume
82Issue
10Page(s)
1402-1406AbstractSouth Asians are among the fastest growing immigrant population groups in the United States. Their traditional diets are rich in minimally processed fruits, vegetables, grains, herbs, and spices. However, the proliferation of ultra-processed foods (highly processed, industrially manufactured formulations) around the globe may compromise the nutrition profile of South Asians, threatening to increase their risk of noncommunicable diseases. This commentary discusses the rise in ultra-processed food consumption among South Asians in the United States and hypothesizes that South Asians may be especially vulnerable to the effects of ultra-processed foods due to their unique cardiovascular disease risk profiles. Using these emerging data, we propose several strategies for preventing the overconsumption of ultra-processed foods among South Asian Americans. These include the implementation of policies to encourage the consumption of whole foods over ultra-processed foods and the development of culturally tailored interventions, which include promoting consumption of traditional diets, improving affordability of healthful, culturally appropriate foods, and cultivating healthier food environments for South Asians living in the United States.‘We know what he likes, even if he doesn’t know’ : how the children of South Asian immigrants characterize and influence the diets of their parents
AbstractAuer, S., Penikalapati, R., Parekh, N., Merdjanoff, A. A., DiClemente, R. J., & Ali, S. H. (n.d.).Publication year
2024Journal title
Health Education ResearchVolume
39Issue
2Page(s)
131-142AbstractForeign-born (first-generation) South Asians face a growing diet-related chronic disease burden. Little is known about whether the adult US-born (second-generation) children of South Asian immigrants can provide unique insights as changemakers in their parents’ dietary behaviors. This study aims to assess how second-generation South Asians describe and influence the dietary behaviors of their parents. Between October and November 2020, 32 second-generation South Asians [mean age 22.4 (SD 2.9), 53% female] participated in online interviews centered around factors involved in their (and their parents) eating behaviors. Thematic analysis revealed three types of parental dietary drivers (socioecological factors that impact the dietary choices of parents): goal-oriented (i.e., parents’ dietary intentionality), capacity-related (e.g., environmental barriers) and sociocultural (cultural familiarity, religion and traditions). Participants described three major mechanisms of influence: recommending new foods, cooking for parents, and bringing new foods home. These influences primarily occurred in the household and often involved participants leveraging their own nutritional knowledge and preferences to expand dietary diversity and healthier behaviors among their parents. Evidence suggests that second-generation South Asians may act as powerful agents of dietary change within their households and can provide novel insights to help address and overcome sociocultural, linguistic, and other structural barriers to better understanding and intervening in the health of the South Asian community.A Multi-Stage Dyadic Qualitative Analysis to Disentangle How Dietary Behaviors of Asian American Young Adults are Influenced by Family
AbstractAli, S. H., Cai, J., Kamal, F., Auer, S., Yang, K., Parikh, R. S., Parekh, N., Islam, N. S., Merdjanoff, A. A., & DiClemente, R. J. (n.d.).Publication year
2023Journal title
Behavioral MedicineAbstractThe dietary behaviors of Asian American (AA) young adults, who face a growing non-communicable disease burden, are impacted by complex socio-ecological forces. Family plays a crucial role in the lifestyle behaviors of AA young adults; however, little is known on the methods, contributors, and impact of familial dietary influence. This study aims to deconstruct the mechanisms of AA young adult familial dietary influence through a multi-perspective qualitative assessment. A five-phase method of dyadic analysis adapted from past research was employed to extract nuanced insights from dyadic interviews with AA young adults and family members, and ground findings in behavioral theory (the Social Cognitive Theory, SCT). 37 interviews were conducted: 18 young adults, comprising 10 different AA ethnic subgroups, and 19 family members (10 parents, 9 siblings). Participants described dietary influences that were both active (facilitating, shaping, and restricting) and passive (e.g., sharing foods or environment, mirroring food behaviors). Influences connected strongly with multiple SCT constructs (e.g., behavioral capacity, reinforcements for active influences, and expectations, observational learning for passive influences). Familial influence contributed to changes in the total amount, variety, and healthfulness of foods consumed. Intra-family dynamics were crucial; family members often leveraged each other’s persuasiveness or food skills to collaboratively influence diet. AA family-based interventions should consider incorporating both passive and active forms of dietary influence within a family unit, involve multiple family members, and allow for individualization to the unique dynamics and dietary behaviors within each family unit.Concordance between Dash Diet and Hypertension : Results from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study
AbstractHussain, B. M., Deierlein, A. L., Kanaya, A. M., Talegawkar, S. A., O’Connor, J. A., Gadgil, M. D., Lin, Y., & Parekh, N. (n.d.).Publication year
2023Journal title
NutrientsVolume
15Issue
16AbstractHigh blood pressure is an important predictor of atherosclerotic cardiovascular disease (ASCVD), particularly among South Asians, who are at higher risk for ASCVD when compared to other population groups. The Dietary Approaches to Stop Hypertension (DASH) dietary pattern is established as the best proven nonpharmacological approach to preventing hypertension in adults. Using data from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) cohort, we calculated a DASH dietary score to examine the association between adherence to the DASH diet and its components, and prevalent and incident hypertension and systolic and diastolic blood pressure, after five years of follow-up. We found that the relative risk ratio (RRR) of incident hypertension was 67% lower among participants in the highest DASH diet score category (aRRR: 0.33; 95% CI: 0.13, 0.82; ptrend = 0.02) compared with those in the lowest DASH diet score category in fully adjusted models. These findings are consistent with previous clinical trials and large prospective cohort studies, adding to evidence that supports the diet-disease relationship established between DASH diet and hypertension. This study is the first to examine DASH diet adherence and hypertension among South Asian adults in the U.S.Development of a Food List to Assess the Diet of South Asians Living in the U.S. : Preliminary Results From a Formative Study
AbstractHussain, B. M., Harris, S., Talegawkar, S. A., Shivakoti, R., Mohsin, F. M., Weiss, R., & Parekh, N. (n.d.).Publication year
2023Journal title
AJPM FocusVolume
2Issue
2AbstractIntroduction: South Asians are an underrepresented population subgroup in the U.S., yet they have higher rates of chronic diseases. There is currently no tool that assesses the nutrition intake of South Asians in the U.S., despite their unique dietary profile that may be associated with disease outcomes. The objective of this preliminary study was to create a food list, inclusive of herbs and spices, that will be used in the development of the web-based South Asian Food Intake System for dietary assessment of South Asian adults living in the U.S. Methods: Authors used a Qualtrics survey to collect sociodemographic information (n=66), and 24-hour diet recall and Home Food Inventory interviews were conducted through Zoom (n=31). Grocery store tours and cookbook and existing food frequency questionnaire review were conducted. Results: A food list of 484 individual food items was generated. These items were sorted into 12 main food categories and condensed into 302 line items. Most respondents (68%) reported consuming South Asian meals regularly and utilizing herbs/spices during food preparation (83%). Conclusions: This pilot study describes the data collection to develop a food list for the South Asian Food Intake System, which can be utilized by educators, clinicians, and researchers to more accurately collect information about dietary intake among South Asian Americans.Dietary Self-Management Using Mobile Health Technology for Adults With Type 2 Diabetes : A Scoping Review
AbstractZheng, Y., Campbell Rice, B., Melkus, G. D., Sun, M., Zweig, S., Jia, W., Parekh, N., He, H., Zhang, Y. L., & Wylie-Rosett, J. (n.d.).Publication year
2023Journal title
Journal of diabetes science and technologyAbstractObjective: Dietary self-management is one key component to achieve optimal glycemic control. Advances in mobile health (mHealth) technology have reduced the burden of diabetes self-management; however, limited evidence has been known regarding the status of the current body of research using mHealth technology for dietary management for adults with type 2 diabetes. Methods: Literature searches were conducted electronically using PubMed, CINAHL (EBSCO), Web of Science Core Collection, PsycINFO (Ovid), EMBASE (Ovid), and Scopus. Keywords and subject headings covered dietary management, type 2 diabetes, and mHealth. Inclusion criteria included studies that applied mHealth for dietary self-management for adults with type 2 diabetes and were published in English as full articles. Results: This review (N = 15 studies) revealed heterogeneity of the mHealth-based dietary self-management or interventions and reported results related to physiological, dietary behavioral, and psychosocial outcomes. Twelve studies applied smartphone apps with varied functions for dietary management or intervention, while three studies applied continuous glucose monitoring (CGM) to guide dietary changes. Among 15 reviewed studies, only three of them were two-arm randomized clinical trial (RCT) with larger sample and 12-month study duration and 12 of them were pilot testing. Nine of 12 pilot studies showed improved HbA1c; most of them resulted in varied dietary changes; and few of them showed improved diabetes distress and depression. Conclusion: Our review provided evidence that the application of mHealth technology for dietary intervention for adults with type 2 diabetes is still in pilot testing. The preliminary effects are inconclusive on physiological, dietary behavioral, and psychosocial outcomes.Evaluating the healthfulness of Asian American young adult dietary behaviors and its association with family structure : Disaggregated results from NHIS 2015
AbstractAli, S. H., Parekh, N., Islam, N. S., Merdjanoff, A. A., & DiClemente, R. J. (n.d.).Publication year
2023Journal title
Nutrition and HealthAbstractBackground: Asian Americans (AA) young adults face a growing non-communicable disease burden linked with poor dietary behaviors. Family plays a significant role in shaping the diet of AA young adults, although little is known on the specific types of family structures most associated with different dietary behaviors. Aim: This analysis explores the changes in dietary behaviors across different AA young adult family structural characteristics. Methods: Nationwide data of 18–35-year-old self-identified Asians surveyed in the 2015 National Health Interview Survey (NHIS) was analyzed. Family structure was measured through family size, family health, and family members in one's life. The Dietary Screener Questionnaire (DSQ) measured the average intake of 10 food and nutrient groups. Published dietary guidelines were used to calculate the number of dietary recommendations met. Results: 670 AA young adults with dietary data were analyzed (26.1% Asian Indian, 26.1% Chinese, 19.3% Filipino, 28.5% other Asian). Participants had an average family size of 2.3. In weighted analyses, 19% of AA young adults met none of the examined dietary recommendations, and only 14% met 3–4 guidelines. Living with a child was associated meeting more dietary recommendations (adjusted odds ratio [AOR]: 1.22; 95%CI: 1.05, 1.42). The adjusted association between living with an older adult and lower odds of meeting dietary recommendations approached significance (AOR: 0.70; 95%CI: 0.49, 1.00). Conclusions: Findings revealed the important role of children and older adults in influencing the diet of AA young adults. Further mixed-methods research to disentangle mechanisms behind the influence of family structure on diet is warranted.Identifying and Estimating Ultraprocessed Food Intake in the US NHANES According to the Nova Classification System of Food Processing
AbstractSteele, E. M., O'Connor, L. E., Juul, F. C., Khandpur, N., Galastri Baraldi, L., Monteiro, C. A., Parekh, N., & Herrick, K. A. (n.d.).Publication year
2023Journal title
Journal of NutritionVolume
153Issue
1Page(s)
225-241AbstractBACKGROUND: The degree of food processing may be an important dimension of diet in how it relates to health outcomes. A major challenge is standardizing food processing classification systems for commonly used datasets. OBJECTIVES: To standardize and increase transparency in its application, we describe the approach used to classify foods and beverages according to the Nova food processing classification in the 24-h dietary recalls from the 2001-2018 cycles of What We Eat in America (WWEIA), NHANES, and investigate variability and potential for Nova misclassification within WWEIA, NHANES 2017-2018 data via various sensitivity analyses. METHODS: First, we described how the Nova classification system was applied to the 2001-2018 WWEIA, NHANES data using the reference approach. Second, we calculated the percentage energy from Nova groups [1: unprocessed or minimally processed foods, 2: processed culinary ingredients, 3: processed foods, and 4: ultraprocessed foods (UPFs)] for the reference approach using day 1 dietary recall data from non-breastfed participants aged ≥1 y from the 2017-2018 WWEIA, NHANES. We then conducted 4 sensitivity analyses comparing potential alternative approaches (e.g., opting for more vs. less degree of processing for ambiguous items) to the reference approach, to assess how estimates differed. RESULTS: The energy contribution of UPFs using the reference approach was 58.2% ± 0.9% of the total energy; unprocessed or minimally processed foods contributed 27.6% ± 0.7%, processed culinary ingredients contributed 5.2% ± 0.1%, and processed foods contributed 9.0% ± 0.3%. In sensitivity analyses, the dietary energy contribution of UPFs ranged from 53.4% ± 0.8% to 60.1% ± 0.8% across alternative approaches. CONCLUSIONS: We present a reference approach for applying the Nova classification system to WWEIA, NHANES 2001-2018 data to promote standardization and comparability of future research. Alternative approaches are also described, with total energy from UPFs differing by ∼6% between approaches for 2017-2018 WWEIA, NHANES.