Niyati Parekh

Niyati Parekh
Professor of Public Health Nutrition
Associate Vice Provost for Faculty Initiatives and Global Engagement, Office of the Provost
-
Professional overview
-
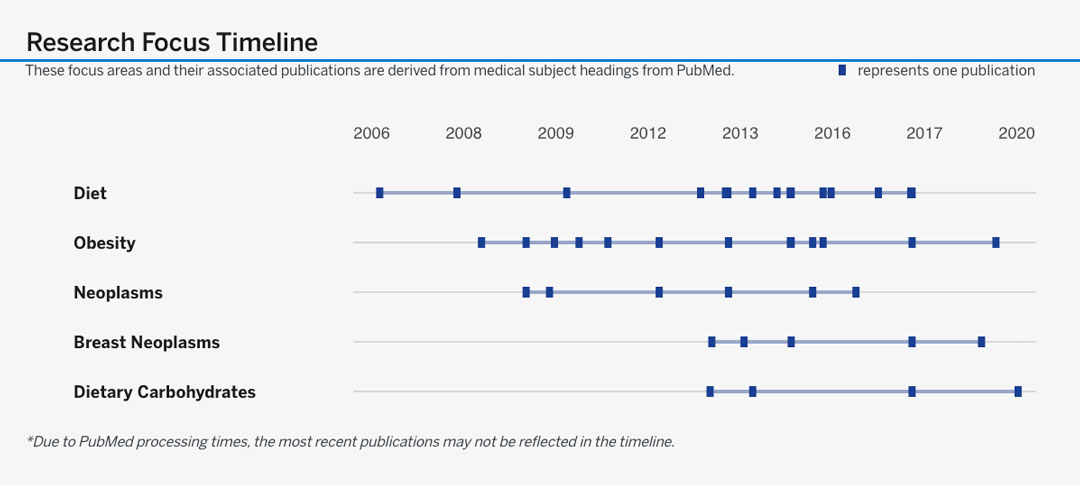
Dr. Niyati Parekh’s research and teaching are motivated by a deep commitment to reduce nutrition-related disease outcomes in at-risk groups. In pursuit of this goal, as a nutritional epidemiologist, she has developed a robust research portfolio that examines the intersection of biological and behavioral factors of non-communicable diseases in US populations. The overarching theme of her research program is to examine the role of nutrition and diet-related factors in the etiology of non-communicable diseases, with a particular focus on obesity, metabolic dysregulation and cancer. Her multidisciplinary research integrates the intricacies from four distinct areas of expertise: disease biology, nutritional biochemistry, epidemiology and biostatistics. She has developed a research program with three interconnected areas that are unified under the theme of investigating diet and non-communicable diseases in populations, using epidemiologic methods. The first arm consists of leveraging existing data to identify dietary patterns, dietary quality and food consumption patterns in populations of interest. The second is to identify dietary determinants and biomarkers that predict disease outcomes including obesity, diabetes, cardiovascular disease and cancer. The third arm is to measure diets using novel dietary assessment methods that will contribute to more accurate and multi-dimensional measurement of diet. The three areas of her work complement each other and reveal preventive measures for populations, inform health policy and guide clinical practice. She has 75 peer-reviewed publications and her work has been supported by awards from the American Cancer Society and NIH.
Dr. Parekh holds an MS in Clinical Nutrition from Mumbai University and a PhD in Nutritional Sciences with a minor in Population Health Sciences from the University of Wisconsin-Madison (2005). After completing a 2-year postdoctoral fellowship in Cancer Epidemiology at the Cancer Institute of New Jersey-Rutgers, she joined New York University Steinhardt’s Department of Nutrition, Food Studies and Public Health in January 2008. With doctoral and postdoctoral training in epidemiological methods, she cross-pollinated the fields of nutrition and public health. In 2015, as Associate Professor of Public Health Nutrition, she transitioned to NYU’s newly launched School of Global Public Health (GPH), as Director of the Public Health Nutrition program (until 2019). She also has an affiliated appointment at the Department of Population Health-Grossman School of Medicine.
Her recent honors include being inducted as a New York Academy of Medicine Fellow, and her appointment as Independent Consultant at UNICEF. She has served the American Society for Nutrition as Chair of the Nutritional Epidemiology Research Group. She teaches graduate courses in the New York Campus and at study abroad sites (Mexico, Abu Dhabi and Florence). Graduate courses taught include Global Nutrition, Nutritional Epidemiology, Perspectives in Public Health and Global Cancer Epidemiology for which she has received awards. Dr. Parekh has served as the Executive Director of Doctoral Programs at GPH since 2017. In this role, she supports about 30 PhD students, and promotes all aspects of their rigorous research and professional development towards impactful careers.
-
Education
-
BS, Life Sciences and Biotechnology, Mumbai University, IndiaMS, Foods, Nutrition, and Clinical Dietetics, Mumbai University, IndiaPhD, Nutritional Sciences (minor Population Health Sciences), University of Wisconsin-Madison, Madison, WI
-
Areas of research and study
-
CancerChronic DiseasesEpidemiologyNutritionObesityPopulation HealthPublic Health Nutrition