
Source: Pew Research Center
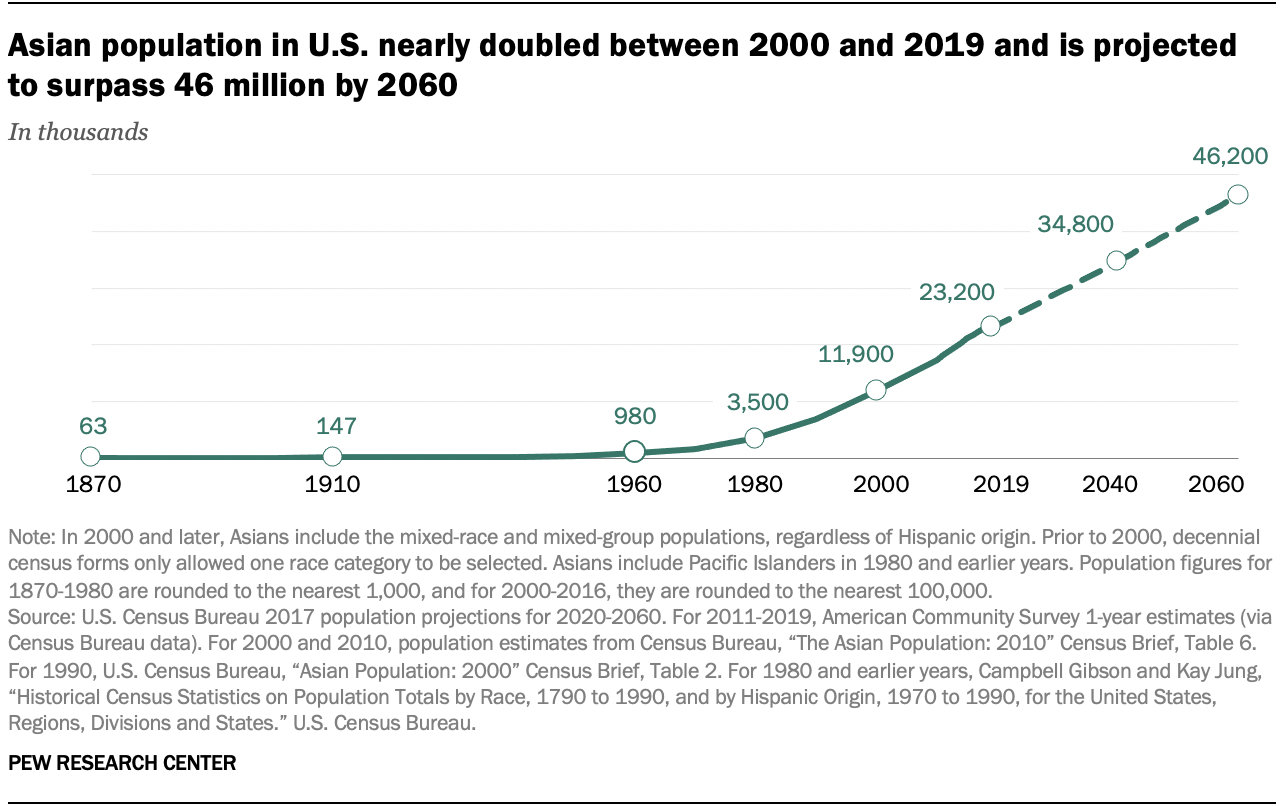
Recent U.S. Census estimates indicate that the Asian American and Pacific Islander (AAPI) population grew almost 95 percent between 2000 and 2019, from nearly 12 million to more than 23 million people, making it the fastest-growing racial/ethnic group in the country. In fact, the population growth of Asians is projected to increase substantially (see Graph 1), and this growth will outpace that of Hispanic/Latino, Black and White populations in the U.S.
Source: Pew Research Center
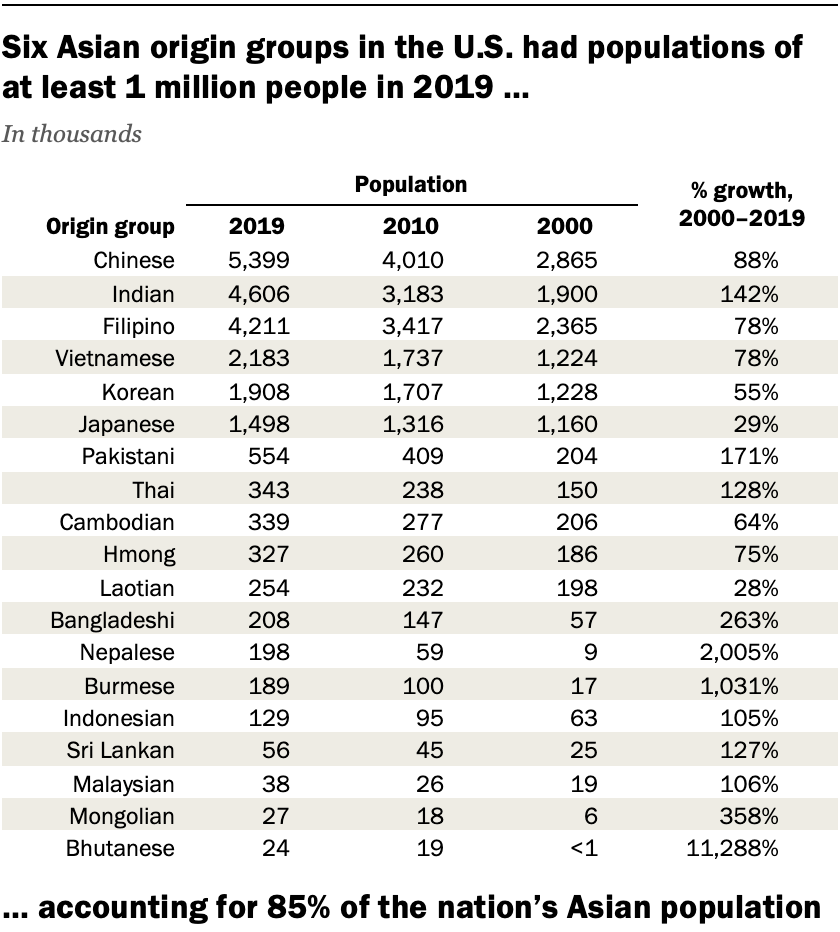
Far from being a monolithic population, Asians come from more than 19 different countries, representing over 50 ethnicities and twice as many languages. While Chinese Americans comprise the largest Asian-origin group (see Table 1), Asian Indians are the second largest, and their growth over the past decade is sizable. Also noteworthy are significant increases in other South Asian origin groups such as Pakistani, Bangladeshi, Nepalese, and Bhutanese.
Source: Pew Research Center
Despite this tremendous population growth, significant health and healthcare disparities remain understudied, and they continue to fuel misconceptions of Asians as the “model minority.” Aggregating all Asians, irrespective of country of origin, into one ethnic group ignores important social, cultural, educational, economic, and health status differences, as well as healthcare needs across distinct ethnic sub-groups.
And yet, national surveys continue to under-sample and under-represent Asian ethnicities. While calls for data disaggregation are not new, the failure to obtain disaggregated data on COVID-19 outcomes masks the disparity in morbidity and mortality experienced across distinct Asian ethnic groups.
Studies show that Black, Hispanic/Latino and American Indian/Alaskan Native populations continue to bear a disproportionate burden of COVID-19 cases, hospitalizations, and mortality. But in states such as New York and California, which have a higher proportion of Asians, COVID-19 hospitalizations and mortality rates across Asian ethnic groups were similar to other communities of color -- not comparable to Whites, which is what is often reported.
A recent retrospective analysis of NYC Health + Hospital data found that from March 1 to May 31, 2020, South Asians had the highest rates of COVID-19 positivity and hospitalizations, second to Hispanic/Latinos and Blacks, respectively. In contrast, Chinese patients had the highest mortality rate of all race/ethnic groups, and were nearly 1.5 times more likely to die than Whites. Added to these disparities in COVID-19 disease burden are anti-Asian discrimination, racism and hate crimes, which are not new but have increased dramatically since the onset of the pandemic. (https://stopaapihate.org/)
We are public health practitioners and educators working to promote equity as a cornerstone of policies related to healthcare access as well as the social and structural determinants of health across communities of color. We call for a greater recognition of the complex histories and experiences of distinct Asian ethnic groups. Without such recognition and action, distinct Asian ethnic groups will remain invisible and health inequities will only widen.

Nina Parikh, PhD, MPH
Clinical Associate Professor of Social and Behavioral Sciences

Farzana Kapadia, PhD, MPH
Associate Professor of Epidemiology

Niyati Parekh, PhD, MS, RD
Executive Director of Doctoral Studies;
Associate Professor of Public Health Nutrition