News articles are written every day exposing health inequities arising from the COVID-19 pandemic; many of them include in-depth analysis using case studies and data. As a consequence of the influx of rapidly changing information about the COVID-19 pandemic, there’s a focus on assessing scientific papers and analyses of health inequalities.
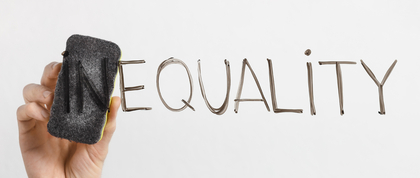
In the first of a series of interactive masterclasses hosted by the NYU Cross-Cutting Initiative on Inequality, GPH associate professor Danielle Ompad showed the class how to recognize bias in scientific papers about the COVID-19 pandemic and strive to avoid it in their own work. She encouraged public health students to “get used to being uncomfortable” in a profession where people will call you out on your biases -- bias being one of the biggest contributors to the unfair treatment of communities of color when it comes to health.
The scientific paper discussed in the session assessed the differential impacts of COVID-19 on Black communities. As explained by Dr. Ompad, health disparities are most commonly evaluated by comparing different data outcomes among different groups of people. In the U.S., groups are most often compared according to race and ethnicity breakdowns. However, there are confounding variables that can impact the results of studies; for instance, the epidemiologists in this study used incomplete census data.
“If racial disparities are inevitable, then how do we close the gap?” inquired one student. Dr. Ompad emphasized the importance of not treating any study group homogeneously when applying the results of case studies to real life scenarios. In the article she examined, the percentage of Black residents who are insured and uninsured, and the socioeconomic heterogeneity among the Black communities studied, are a few variables that inadvertently influenced results.
It’s important for public health professionals to realize that current societal norms continue to foster health inequities that have persisted for decades in Black communities. For example, white patients are still reportedly more likely to receive treatment for pain than African-American patients as a result of past biases about African-Americans and pain tolerance.
Policies can be difficult to change, but the work being done every day to dispel misinformation is just as important. Ultimately, whether you’re working in the global public health field or not, Dr. Ompad asked, “What can we do in our own lives to keep our biases in check when it comes to health disparities and inequality? For instance, instead of convincing people that the coronavirus vaccine is safe, we need to figure out what did we [healthcare professionals] do to make people think it isn’t safe.”
Author
Destine Manson
GPH Communications Editorial Assistant